“You’re Not Dealing With A Mineral, But A Condition That Has To Be Treated Uniquely”
There are several steps that has to be taken in order to achieve adequate serum sodium levels without any complications:
STEP 1: Measure Osmolality !
HYPERTONIC hyponatremia ( >295 )
in simple terms; this is when molecules of high osmolarity drags water in causing dilution of serum Na+ (if your patient is receiving mannitol, or hyperglycemic)
Quick Tip: In cases of hyperglycemia you can calculate correction this way: for every 100 increments of serum glucose above 200 mg/dl, there is a 2 meq decrement in serum sodium 🙂
NORMOTONIC hyponatremia ( 275-295 )
hyperlipidemia, hyperphosphatemia masks some of the serum cations including sodium (lab miscalculations).
HYPOTONIC hyponatremia ( <275 )
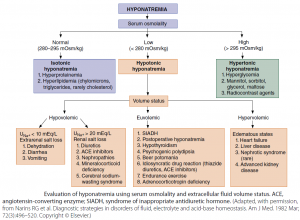
there is a true loss of sodium, were you need to investigate the cause according to clinical scenario and urine sodium levels. (algorithm attached below)
STEP 2: Treat Reversible Causes
Identifying the cause of hyponatremia is an important step as it helps in the management of the patient’s condition as a whole and prevent complications led by the infusion of extra saline. Different causes of hyponatremia can be recognized through clinical scenario and urine sodium levels. (algorithm attached below)
some of the reversible causes commonly encountered in critical care are:
Hypovolemia:
Aside from hypovolemia being a direct cause of hyponatremia (as there is an extra renal loss of sodium and an increase in insensible loss of sodium), another factor taking part of hyponatremia is ADH compensation.
ADH drags more water in to compensate for hypovolemia leading to further (dilutional) reduction in serum sodium Once volume repletion happens, ADH is suppressed and sodium levels increase.
Adrenal Insufficiency:
Starting patients with suspected adrenal insufficiency on corticosteroids would stimulate angiotensin and aldosterone to return Na+ back to its normal levels.
hydrocortisone 100mg 6 hourly + fludrocortisone 0.1 mg 3 times per week
Medication Side Effects:
Certain medications side effect could be the reason behind unexplained hyponatremia (mono-antipsychotic therapy,
thiazide diuretics, etc.).
Ceasing these offending medications can it self lead to an increase in serum sodium without the need of any saline infusion.
SIADH:
If it’s confirmed or suspected start the patient on tolvaptan PO 15mg 24 hourly, and check serum sodium frequently.
ICU Tip: if vaptans are not available it’s a better idea to use hypertonic saline instead of 0.9% saline as the latter has a lower osmolality (more free water, less sodium) therefore, worsens SIADH.
Hypokalemia:
If serum K+ is low, replenishing it would lead to an appropriate increase in serum sodium.
as potassium is mainly intracellular It would exchange with intracellular Na+ through designated channels which will cause outward shifting of sodium into extracellular spaces (including blood vessels!)
Step 3: Is it Mild, Moderate, or Severe?
Mild Hyponatremia (130-135):
usually responds to per oral fluid / intravenous hypotonic fluid (D/W) restriction and simply treating any of the reversible causes. (explained above)
Moderate Hyponatremia (120-130):
– If patient is symptomatic (coma, seizures) or with brain pathology (acute CVA, brain tumor, encephalitis):
it should be treated quickly with 50ml of 3% saline in order to prevent further increase in ICP and the risk of brain herniation.
did you know: patients with a brain pathology is better kept hypernatremic than normonatremic!
– If asymptomatic moderate hyponatremia:
it should be treated as same as mild hyponatremia (fluid restriction and reversal of factors) with additional saline infusion if former measures aren’t efficient enough.
Severe Hyponatremia (<120):
– if patient is symptomatic:
150 ml of 3% saline should be given in 20 minutes, if symptoms remain another 150 ml is to be given (300 ml of 3% saline are found to increase sodium 6 meq).
– If patient isn’t seriously symptomatic:
patient’s serum sodium levels should be corrected slowly; ensuring a correction of 6-8 meq in 24 h via Madias equation. (if serum sodium is lower than 110 it is safest to not increase sodium > 5 meq per 24 hour)
Adrogue Madias Equation (how to calculate rate of fluid ml/hour):
1000 * meq/h change of sodium * (TBW + 1)
—————————————————————
infustated fluid sodium – serum sodium
TBW= KG * 0.6 (female) or 0.5 (male)
Meq/h change of sodium= 8 meq divided over 24h = 0.33 meq/h
Infusated fluid sodium = in 1L of 3% saline there is 514meq
in 1L of 0.9% saline there is 154meq

Step 4: Prevent Overcorrection:
In severe hyponatremia estimated correction rate can sometimes be exceeded and this puts the patient at risk of developing neurological complications such as “Osmolar Demyelination Syndrome” which results of osmotic stress in a period shorter than brain’s ability to adapt.
Risk Factors of ODS Include:
1) sodium level < 105-110 meq/dl
2) malnutrition
3) hypokalemia
4) alcoholism
5) liver cirrhosis
How to prevent overcorrection?
1) Measure serum sodium 1-3 hourly as all of made equations are not 100% accurate.
2) Recognize reversible causes and treat first before correcting sodium levels with any fluids.
2) Recognize patients at risk and start prophylactic S/C desmopressin 1-2 mcg 8 hourly.